To Bleed or Not To Bleed
Menopausal Women Taking Hormones Do Not Necessitate Menstrual Cycling
The hot topic for celebrity talk shows and celebrity books is bioidentical hormones. The media has highlighted the term “bioidentical hormones” thereby making it a familiar subject for both women and men, especially those coming to grips with the aging process. Now we can further define the term “natural” and specify & “bioidentical” which gives everyone a new understanding and appreciation for hormone replacement.
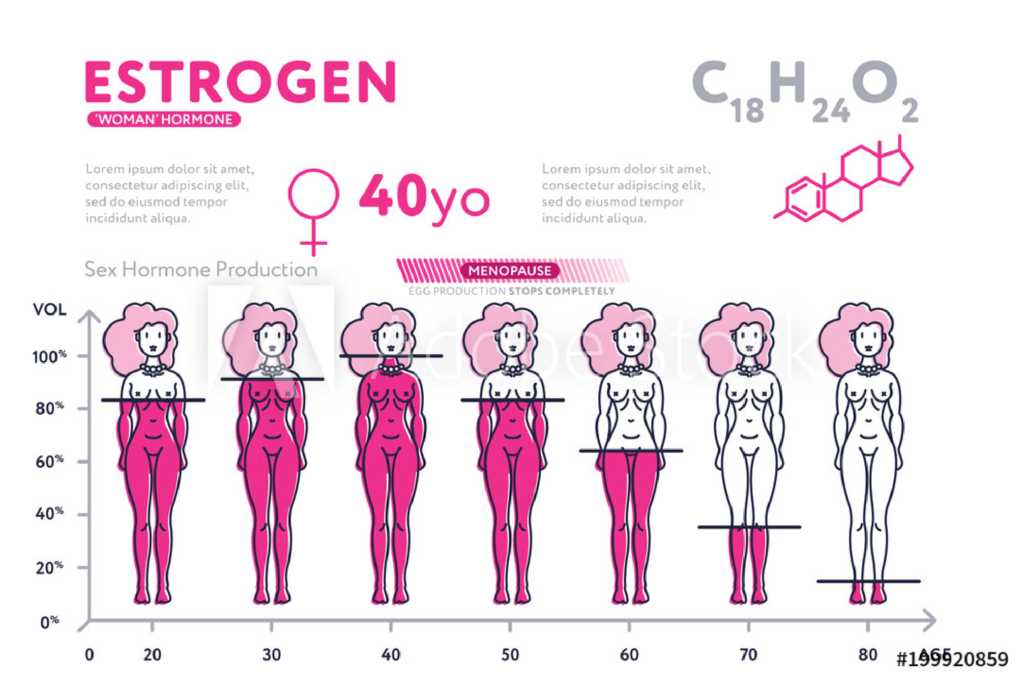
Out of this media frenzy have emerged new “experts” with “expert” opinions on the right way to take hormones. One of these “expert” methodologies of hormone replacement unfortunately has made many women apprehensive. Some are so displeased that they avoid taking hormones altogether. Some experts theorize that cycling (creating a period every month) is recommended and natural. The implication is that women menstruate while they are “young” and healthy. In order to maintain that same healthy status all menopausal women should continue to menstruate. This “cycling” is done by stopping progesterone for one week of each month and thereby creating a menstrual cycle. Most women find this recommendation unsatisfactory. If women believe that taking hormones requires that they have a period, most women choose to pass on hormone replacement.
What is cycling? It is the fall of women’s hormones that results in menstruation. If a woman stops the progesterone for a few days every month she will cycle and bleed. This is possible even if you have been years without a period, unless, of course, you have had a hysterectomy. Just because it is “natural” in younger women does not mean it is necessary or beneficial for menopausal women.
First of all, hormone replacement therapy does not put one in a state of pregnancy. During pregnancy the levels of estrogen might be in the hundreds. On estrogen replacement, ideal estradiol levels are typically 60-100 pg/dl, far from that seen in pregnancy.
Secondly, the reason a woman menstruates is to clean the uterus in preparation for the eventual implantation of a fertilized egg. If one is not interested in becoming pregnant, there is no physiologic reason or benefit to menstruate.
A recent article in the Obstetric/Gynecological literature claimed that unexpected vaginal bleeding was the most common reason women stopped taking HRT. The cessation of periods was one thing that women welcomed with menopause. The medical literature often addresses how to stop and prevent postmenopausal vaginal bleeding so that women will be comfortable in continuing HRT. We advocate increasing progesterone to prevent post-menopausal bleeding. With the appropriate balancing of estrogen and progesterone, women should not bleed and will be more satisfied with continuous use of HRT. Also, since estrogen and progesterone are so important, why take them for only three weeks per month and stop them to bleed in the fourth week? A woman would lose the protection and benefit of estrogen and progesterone for 25% of the time.
For years, women have been treated with birth control pills taken continuously and not cycled to control PMS. It is the fall of women’s hormones that takes place right before their periods that causes the symptoms of PMS. By taking birth control pills continuously, a woman can avoid this drop of hormones and the symptoms of PMS. The pharmaceutical industry has now caught onto this and promotes a new birth control pill that is cycled for bleeding only every four months instead of monthly. The researchers claim that while no menstruation is necessary, the cycling allows women to menstruate every four months to make them feel more “normal.” We now realize that even pre-menopausal women do not need to menstruate, let alone post-menopausal women.
Remember, cycling involves stopping the hormones for a week each month. Another reason not to cycle is the loss of protection that takes place when the progesterone is not present. Bioidentical progesterone protects the breasts and uterus against cancer. The bleeding that takes place with menstruation is not what protects the uterus against cancer. It is the direct effect of progesterone on the uterus that protects it. Stopping progesterone for a week means that the body is without the protective benefits of progesterone for those days. It makes no sense to lose the important protective benefits for seven days every month.
Recent studies have shown that Provera (medroxy-progesterone) increases the risk of breast cancer and increases the thickening of the breast tissue. It does this by direct stimulation (up regulation) of estrogen receptor sites in the breast. One study showed that Provera increased breast stimulation by 400% over baseline. The same study showed that bioidentical progesterone (different from Provera), does not stimulate breast tissue as it down regulates receptor sites in the breast. Therefore, why lose this protective effect of progesterone by stopping it for 25% of the month which means you lose 25% of the protection? There is a condition known as “endometrial hyperplasia.” This condition causes increased thickening of the endometrial stripe (uterine lining) which is a precursor to cancer. This condition must be treated to avoid the development of cancer. The treatment is high dose progesterone (or Provera by conventional physicians) to shrink this tissue. If repeat ultrasound does not show a decrease in endometrial lining, then the dose of progesterone is doubled. The shrinkage of the endometrial tissue is a result of the direct stimulation by progesterone. The protection does not occur because of the shedding of the lining. A constant sufficient dose of progesterone is the better protection against cancer. Progesterone should never be stopped for any reason!
In summary, women on hormone replacement therapy do not need to cycle (stop the progesterone) and bleed on a periodic basis. There is no substantiated benefit to the body to regularly bleed. And it certainly makes hormone replacement therapy and its many protective benefits a more attractive and convenient regimen for women.